DIVERTICULAR DISEASE
What is diverticular disease?
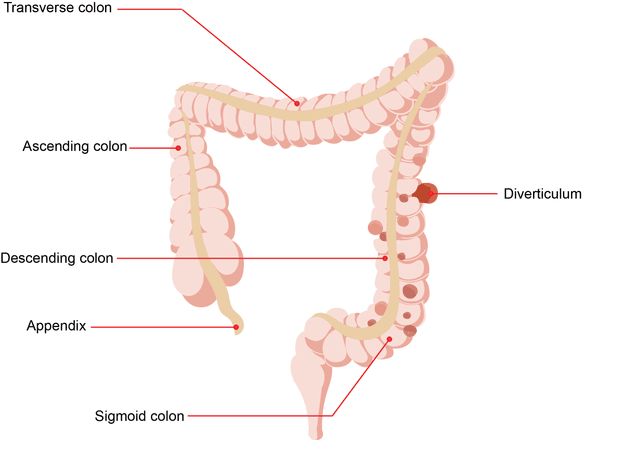
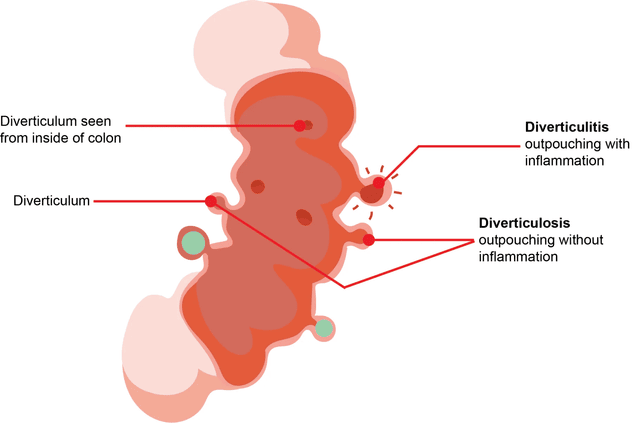
Diverticular disease is a common condition where small pockets or outpouchings (single - diverticulum, multiple - diverticula) form in the wall of the large bowel.
Who is at risk of developing diverticular disease?
Around 1 in 3 Australians over the age of 45 have diverticular disease. Many are unaware they have it.
The main risk factor for diverticular disease is a low fibre diet. Less fibre increases constipation and results in harder compact stools which require more pressure to push them along the large bowel. This pressure may lead to ‘blow-outs’ and formation of pockets. People who eat a high fibre diet are much less likely to develop diverticular disease.
What problems can diverticular disease cause?
Diverticulosis
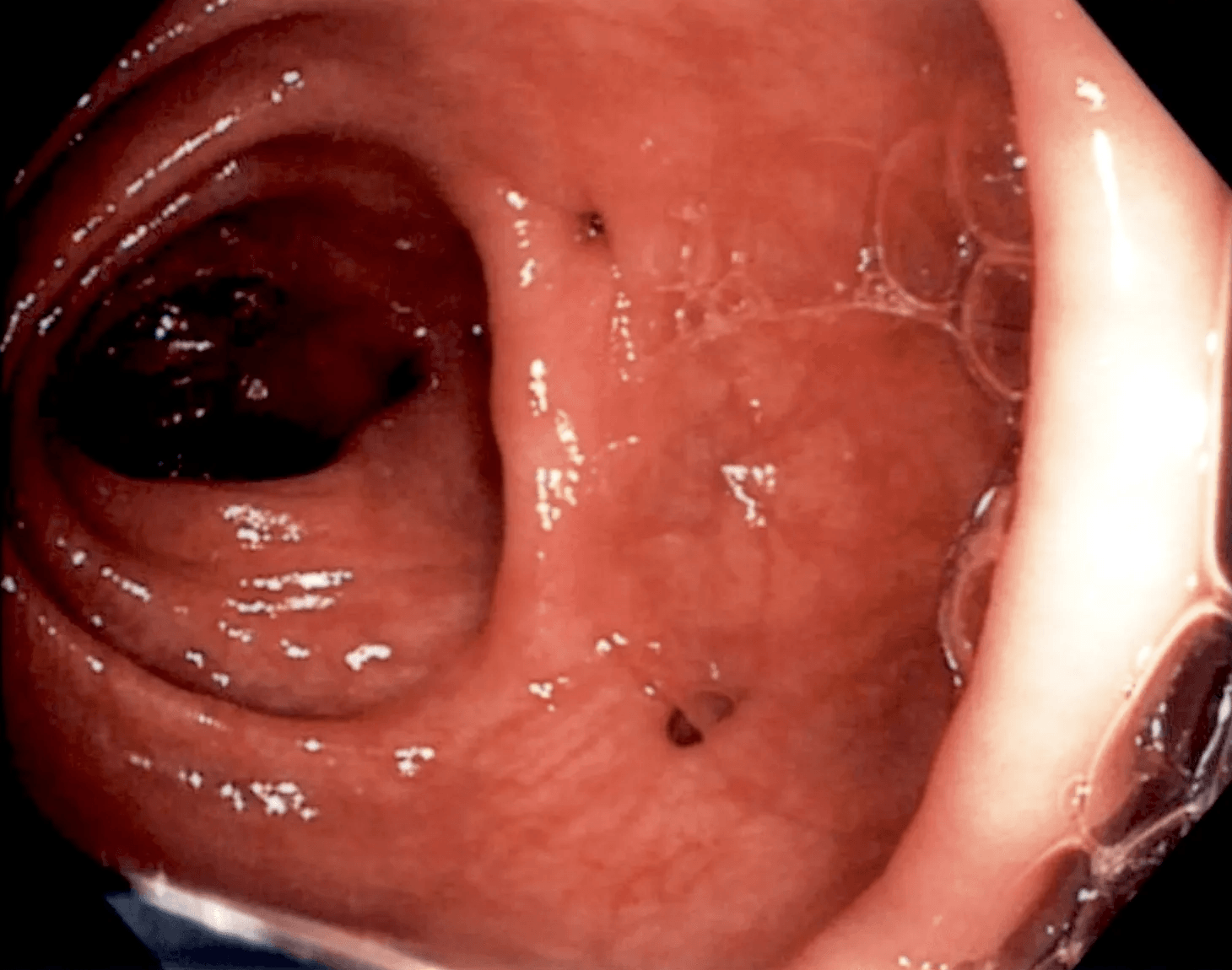
Diverticulosis is the condition of having diverticula that are not inflamed or infected. Around 1 in 3 people with diverticulosis develop symptoms and complications. Symptoms may include mild cramps, bloating, constipation or diarrhoea. Diverticulosis is usually diagnosed during colonoscopy for bowel cancer screening or investigation of bowel symptoms.
Diverticulitis
Diverticulitis occurs when the diverticula becomes inflamed or infected. The severity of symptoms depends on the extent of the infection and complications. The most common symptom of diverticulitis is constant abdominal pain in the lower left side of the abdomen. It is also associated with changed bowel habits such as constipation or diarrhoea. Infection may cause fever, nausea and vomiting. Diverticulitis is usually diagnosed on a CT scan.
Other serious complications of diverticular disease include bleeding, bowel obstruction (blockage), bowel perforation leading to abscess formation inside the abdomen and fistula formation to other nearby organs such as the bladder.
How is diverticulitis treated?
For mild diverticulitis, you may be treated at home with bowel rest by having a low fibre or fluid only diet. You may be prescribed antibiotics and mild painkillers.
For severe diverticulitis, you may need to be admitted into hospital and be given antibiotics and fluids through your vein and stronger painkillers. Most people improve with treatment. However, people who do not improve with treatment or who develop serious complications may require emergency surgery.
How can diverticular disease be prevented?
A high fibre diet (30 grams per day) helps to prevent constipation and formation of diverticula. The diet must include good quantities of roughage such as fruits (e.g. apples and pears), vegetables and wholegrain cereals. Baked beans and legumes are also high in fibre. A fibre supplement or unprocessed wheat bran can increase fibre intake and provide an additional 4 to 6 grams of fibre each day.
Drinking enough water (up to 8 cups per day) and exercising regularly are also recommended.
Related Information